Neuroendocrine tumors (NETs) have been on the rise in recent years, and among them, pancreatic neuroendocrine tumors (PanNETs) pose a significant health concern. However, a recent Cell Death and Disease study offers hope in the fight against these tumors. This groundbreaking research explores the effects of a ketogenic dietary intervention on the onset and progression of PanNETs, shedding light on a potential therapeutic approach.
Pancreatic Neuroendocrine Tumors: A Growing Concern
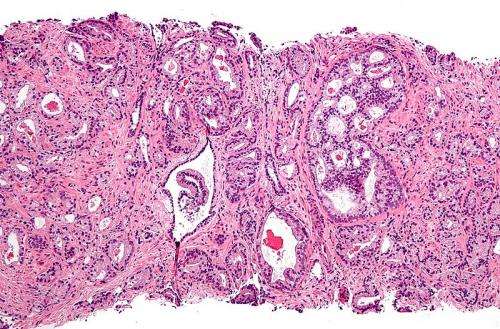
PanNETs, a subtype of NETs, are rare but have become increasingly prevalent. These tumors originate from pancreatic islet cells and can be functional or non-functional. While functional PanNETs produce hormones that lead to hormone syndromes, non-functional PanNETs, which comprise most cases, do not exhibit these characteristics.
The progression of PanNETs often involves the development of liver metastases, making them challenging to treat. Traditional treatments have shown limited success in shrinking these tumors, emphasizing the need for innovative interventions.
Understanding the Role of Insulin
The study draws attention to the role of insulin in PanNET development. Both human and mouse models have revealed a connection between elevated insulin levels and increased tumor growth. Conversely, reducing insulin levels has been associated with decreased tumor development.
Enter the Ketogenic Diet
The ketogenic diet, known for its low carbohydrate and high-fat composition, has gained recognition for its potential health benefits. In the context of cancer, previous research has suggested that a ketogenic diet can lower insulin levels without adverse effects.
In this study, researchers fed a ketogenic diet to mice with non-functional PanNETs using a Pancreatic β-cell-specific Men1 deficient mouse model. The results were promising.
Ketogenic Diet: A Game Changer
The findings demonstrated that a ketogenic diet could significantly suppress the onset and progression of non-functional PanNETs in the mouse model. What is more, this dietary intervention also had a positive impact on pituitary NET development in the mice.
The Implications for Human PanNET Patients
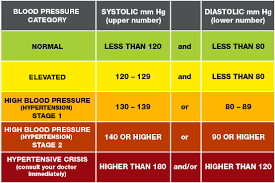
These results open up exciting possibilities for PanNET patients. High blood glucose levels have been associated with poorer outcomes in PanNET patients, especially those undergoing chemotherapy. Metformin, a blood sugar-reducing drug, has shown promise in improving chemotherapy effects for PanNET patients.
Therefore, reducing blood glucose levels through a ketogenic diet could enhance the prognosis for human PanNET patients. This treatment approach also holds promise for other cancers that rely on the insulin-regulated PI3K-Akt-mTOR pathway.
In conclusion, this study offers hope in the battle against PanNETs and potentially other NETs. The ketogenic diet’s ability to suppress tumor progression in a mouse model suggests a novel therapeutic intervention that could benefit patients in the future. Further research is needed, but this study paves the way for innovative approaches to combating neuroendocrine tumors.
Using the ketogenic diet as a therapeutic intervention for PanNETs may have potential side effects. However, it is essential to note that this research is still in its early stages, and further human studies are needed to understand the risks thoroughly. Some potential side effects of the ketogenic diet may include:
- Keto Flu: When transitioning to a ketogenic diet, some people experience “keto flu” symptoms, including fatigue, headaches, nausea, and dizziness.
- Nutritional Deficiencies: A restrictive diet may lead to nutritional deficiencies, especially if not carefully planned. Monitoring vitamin and mineral intake is crucial.
- Gastrointestinal Issues: Constipation and diarrhea can occur due to changes in dietary fiber and fat consumption.
- Liver and Kidney Function: There are concerns about how the diet may affect liver and kidney function, as they play a role in metabolizing ketone bodies.
- Increased Cholesterol Levels: Some individuals may experience increased cholesterol levels when on a high-fat diet, which could pose cardiovascular risks.
- Bone Health: The ketogenic diet may impact bone health due to its potential for calcium loss.
Regarding the use of Metformin, it is generally considered a safe and well-tolerated medication. However, like any medication, it can have side effects. Common side effects of Metformin may include gastrointestinal symptoms such as diarrhea, nausea, and abdominal discomfort. In some cases, it may also lead to vitamin B12 deficiency or, rarely, a serious condition called lactic acidosis. The risk of side effects should be weighed against the potential benefits of Metformin as part of PanNET treatment.
The following steps in research to determine the effectiveness of the ketogenic diet in human PanNET patients involve conducting clinical trials. These trials would involve carefully controlled studies on human participants to assess the diet’s impact on tumor growth, blood glucose levels, and overall health. Researchers would monitor for potential side effects and evaluate the diet’s efficacy in improving patient outcomes.
Additionally, research may explore the combination of a ketogenic diet with other treatment modalities, such as chemotherapy or targeted therapies, to determine if synergistic effects could enhance the treatment of PanNETs. Ultimately, conducting well-designed clinical trials will be essential to providing more concrete evidence of the diet’s effectiveness and safety in humans.
Cited Works:
Barrea, Luigi, Sara Cacciapuoti, Matteo Megna, Ludovica Verde, Claudio Marasca, Rosa Vono, Elisabetta Camajani, et al. “The effect of the ketogenic diet on Acne: Could it be a therapeutic tool?.” Critical Reviews in Food Science and Nutrition (2023): 1–20.
Cohen, Yotam, Rafael Valdés-Mas, and Eran Elinav. “The Role of Artificial Intelligence in Deciphering Diet–Disease Relationships: Case Studies.” Annual Review of Nutrition 43 (2023).
Rana, Avinash, and Monika Arora. “Ketogenic diet: Assessing YouTube video information using quality, reliability, and text analytics methods.” Nutrition and Health (2023): 02601060231193789.